Understanding Crohn's Disease: Symptoms, Causes, and What to Expect in 2025
Crohn’s disease is a chronic condition that affects millions. This guide explores the symptoms of Crohn’s disease, including how it manifests in females, the stages of active Crohn’s, and what to expect when living with this condition. View real-life Crohn’s disease pictures and learn about treatment options
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
Crohn’s disease, a type of inflammatory bowel disease (IBD), presents a significant challenge for individuals and healthcare providers alike. It is characterized by chronic inflammation of the digestive tract, which can lead to abdominal pain, severe diarrhea, fatigue, weight loss, and malnutrition. The exact cause of Crohn’s disease is not fully understood, but it is believed to involve a combination of genetic predisposition, immune system dysfunction, and environmental factors. Unlike ulcerative colitis, another form of IBD, Crohn’s can affect any part of the gastrointestinal tract and often appears in patches of inflammation alongside healthy tissue.
How Crohn’s Disease Affects the Body
Crohn’s disease primarily impacts the digestive system, causing inflammation that can lead to significant damage over time. This inflammation can result in ulcers, strictures (narrowing of the bowel due to scar tissue), and fistulas (tunnels that can form from the intestine to other organs or the skin). Beyond the digestive tract, Crohn’s can also manifest with extraintestinal symptoms, affecting joints, skin, eyes, and the liver. For instance, individuals may experience arthritis, skin rashes like erythema nodosum, or eye inflammation such as uveitis. The chronic inflammation can also lead to systemic issues like anemia, nutrient deficiencies, and osteoporosis, highlighting its widespread impact on overall bodily health and function.
Symptoms of Crohn’s Disease in Females
While many symptoms of Crohn’s disease are similar across all genders, some aspects may present uniquely or be particularly impactful for females. Common symptoms include persistent diarrhea, abdominal pain and cramping, blood in stool, fatigue, and unexplained weight loss. However, females may also experience specific challenges related to reproductive health, such as menstrual irregularities, reduced fertility, or complications during pregnancy. The disease and its treatments can influence bone density, increasing the risk of osteoporosis, which is a concern particularly for women. Additionally, the psychological burden of a chronic illness, including body image issues and social impact, can be pronounced.
What to Expect with Active Crohn’s Disease
During periods of active Crohn’s disease, often referred to as flares, individuals typically experience an intensification of their symptoms. This can include severe abdominal pain, frequent and urgent bowel movements, sometimes with blood, fever, and extreme fatigue. Flares can be unpredictable in their onset and severity, significantly disrupting daily life. Complications like bowel obstructions due to strictures, abscesses, or fistulas may require urgent medical intervention. Managing active Crohn’s often involves a combination of medication, dietary adjustments, and close monitoring by a healthcare team to bring the inflammation under control and induce remission.
What Crohn’s Disease Imaging Can Show
Imaging techniques play a crucial role in diagnosing Crohn’s disease, assessing its extent, and monitoring its progression. Endoscopic procedures like colonoscopy and upper endoscopy allow direct visualization of the intestinal lining and enable biopsies for microscopic examination. Magnetic resonance imaging (MRI) and computed tomography (CT) scans can reveal inflammation, strictures, fistulas, and abscesses both within and outside the bowel. MRI enterography is particularly useful for evaluating the small intestine without radiation exposure. These images provide vital information that helps clinicians determine the specific areas affected, the severity of the disease, and guide treatment decisions, illustrating the internal changes characteristic of Crohn’s.
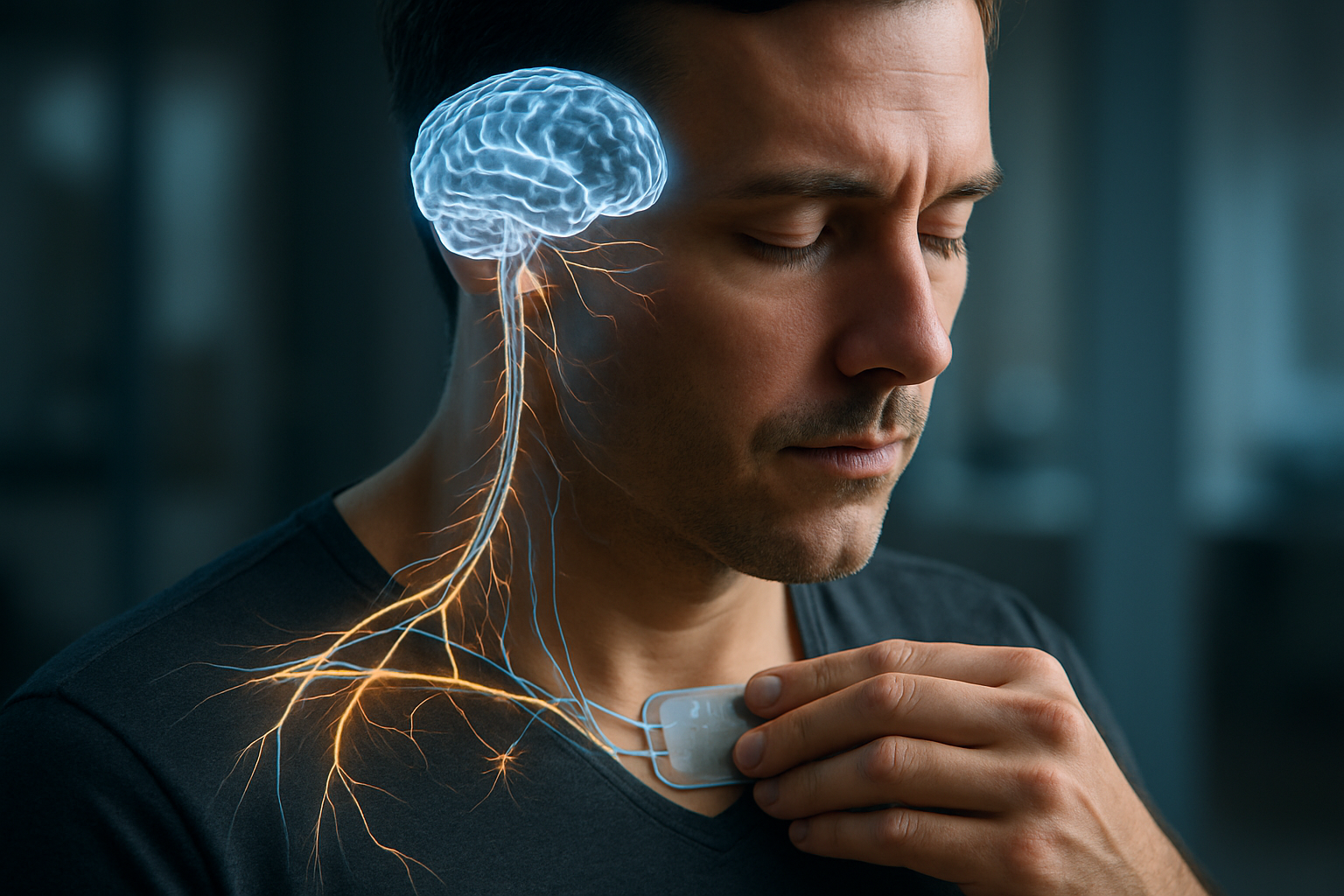
Treatment Options and Expected Advances by 2025
Treatment for Crohn’s disease aims to reduce inflammation, relieve symptoms, and achieve long-term remission, thereby improving quality of life. Current treatment options include anti-inflammatory drugs, immune system suppressors, and biologic therapies. Biologics, such as anti-TNF agents, work by targeting specific proteins involved in the inflammatory process and have revolutionized treatment for many individuals. Surgical interventions may be necessary to remove damaged sections of the bowel, close fistulas, or widen strictures, though surgery is not a cure. Looking towards 2025, research continues to explore new therapeutic targets and personalized medicine approaches. Advances are expected in novel biologic and small molecule drugs with different mechanisms of action, offering more options for those who do not respond to existing treatments. There is also a growing focus on precision medicine, using genetic and molecular markers to predict treatment response, potentially leading to more tailored and effective therapies for individuals with Crohn’s disease.
Crohn’s disease is a chronic condition that requires ongoing management and a personalized approach to care. While there is currently no cure, significant progress in understanding its mechanisms and developing effective treatments has greatly improved outcomes for many individuals. Continuous research and medical advancements offer hope for even more targeted and successful therapies in the years to come, further enhancing the quality of life for those living with this condition. Early diagnosis and a strong partnership with healthcare professionals remain key to navigating the complexities of Crohn’s disease.




