Screwless Versus Screw-Based Dental Implants 2026
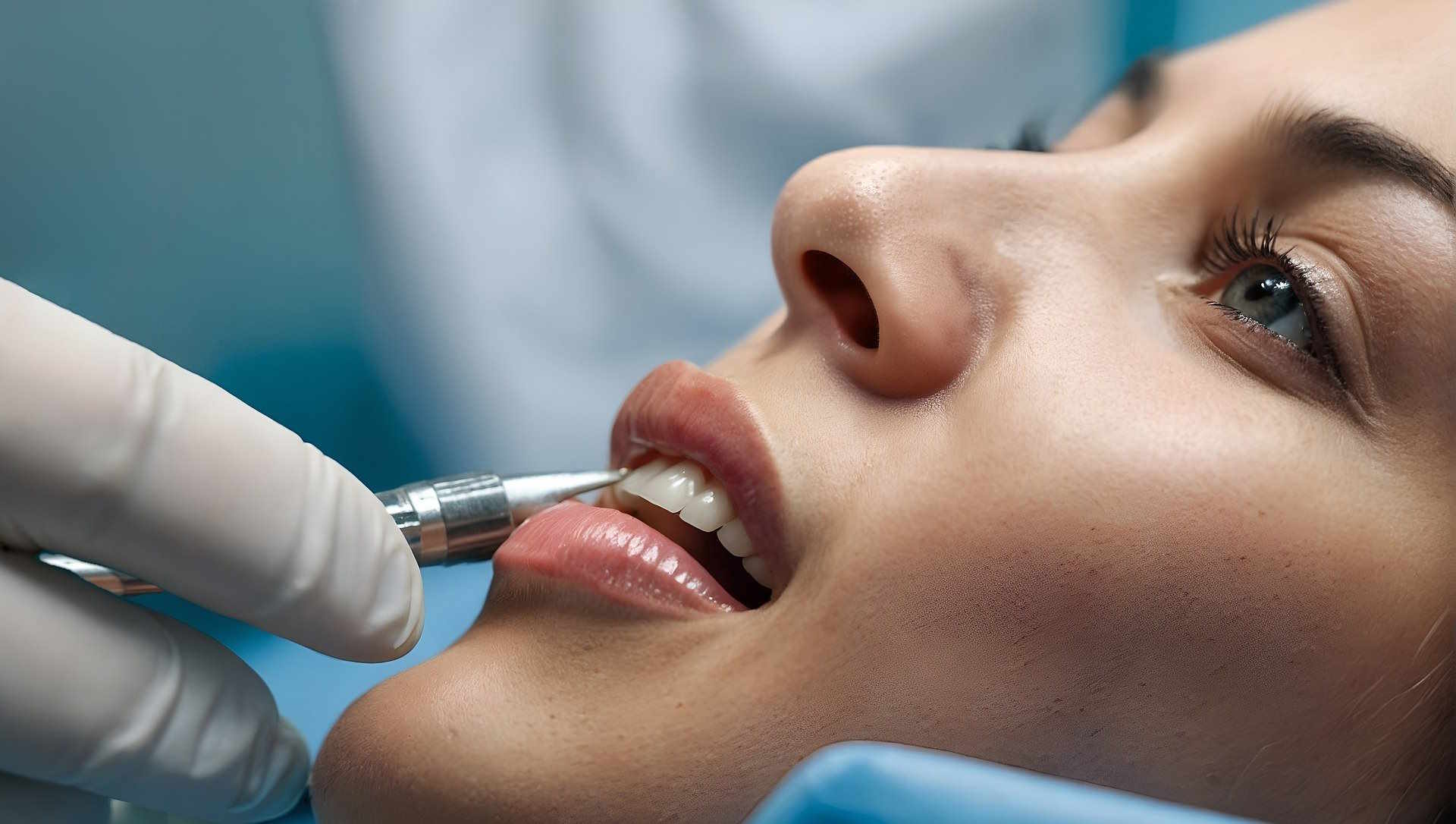
In 2026, dental implants in the U.S. include screwless and screw-based systems, each with unique design features impacting surgery, healing, maintenance, and aesthetics. Knowing these differences helps patients and clinicians choose the best tooth replacement method for individual needs.
Overview of Screwless Dental Implants
Screwless dental implants, also referred to as cement-retained or press-fit implants, consist of a one-piece or two-piece design where the prosthetic tooth is attached without the use of visible screws. Instead of a screw-thread connection, they typically utilize friction fit or dental cement to secure the abutment and crown to the implant post. This design eliminates the screw access hole often seen in traditional systems, which may benefit aesthetic outcomes, especially in the anterior (front) smile zone.
These implants rely on surface treatments that encourage osseointegration, the biological process where bone cells attach directly to the implant surface, securing its stability within the jawbone. The placement involves preparing a precise socket in the bone to receive the implant. Once integrated, the crown is bonded or pressed into place, completing the restoration.
Description of Screw-Based Dental Implants
Traditional screw-based dental implants involve multiple components: a titanium or titanium-alloy screw placed surgically into the jawbone, an abutment connected via a smaller screw, and a prosthetic crown secured atop. This modular system allows for removal or replacement of the prosthetic components without affecting the implant embedded in bone.
The threaded design ensures primary stability at placement and facilitates osseointegration during healing. After sufficient bone integration, the abutment and crown are attached, allowing for some flexibility in prosthetic adjustments or maintenance.
Surgical Procedures and Treatment Phases
Both screwless and screw-based implants require an initial surgical procedure where the implant post is placed into the jawbone. This often involves local anesthesia and sometimes sedation, with the site prepared through incisions in the gum tissue. Following implant placement, a healing period of several months allows for osseointegration.
Screw-based implants generally involve more steps during prosthetic restoration, as the abutment and crown are separate components fixed by screws. Screwless systems may streamline this by integrating the abutment and crown or bonding them via cement.
Healing Process and Infection Considerations
Healing times vary depending on factors such as patient health, jawbone quality, and surgical technique. Both systems require osseointegration periods commonly ranging from 3 to 6 months.
One consideration with screw-based implants is the potential presence of a micro-gap at the implant-abutment interface where screws connect. This small gap may harbor bacteria, potentially increasing risk of peri-implantitis (inflammation around the implant) and affecting soft tissue health. Careful hygiene and regular dental follow-up are important.
Screwless implants aim to reduce these micro-gaps due to their design, potentially lowering bacterial colonization at the interface. However, current research is inconclusive on long-term differences in infection rates between the two types.
Maintenance and Longevity
Maintenance of dental implants involves regular dental check-ups and oral hygiene practices to prevent complications. Screw-based systems permit easier access to the abutment and crown connections for repairs or replacements without disturbing the implant fixture itself.
Screwless designs, by integrating components or using cemented connections, may complicate prosthetic retrieval if repairs are needed. Cement retention also carries a risk of excess cement causing irritation and inflammation if not properly managed.
Both types demonstrate high success rates, with most implants lasting 10 to 20 years or more when properly maintained.
Aesthetic Considerations
Aesthetics is a key factor, particularly for front teeth replacement. Screwless implants eliminate visible screw access holes, contributing to a smoother gum-to-crown transition and natural appearance.
Screw-based implants require small access openings for screws, which are filled with composite material or healing caps, but may sometimes compromise the translucency or uniformity of the prosthesis. Advanced techniques and materials have improved these outcomes, minimizing aesthetic differences.
Patient Suitability
Patient-specific factors influence the choice between screwless and screw-based implants. Screwless implants are often selected when improved aesthetics are prioritized and in cases where a simplified prosthetic connection is desirable.
Screw-based implants may be favored for their modularity, ease of prosthetic management, and suitability in complex rehabilitations or patients with higher risk of implant complications.
Typical Costs in United States (2026)
When considering dental implant systems in the United States, typical price ranges vary based on implant type, complexity, and geographic location:
-
Basic option (screwless or simpler implants): Approximately $1,500 to $2,500 per implant. This typically includes implant placement and a cement-retained prosthetic crown suitable for single-tooth replacement in non-complex cases.
-
Standard option (traditional screw-based implants): Around $2,000 to $3,500 per implant. This price range usually covers multi-piece implant systems with screw-retained crowns, allowing for greater prosthetic versatility.
-
Premium option (advanced systems with specialized components): $3,500 to $5,000 or more per implant. These may incorporate custom abutments, bone grafting procedures, or premium materials suited for complex restorations.
Costs depend on individual clinical factors including bone quality, the need for additional procedures such as sinus lifts, and prosthesis type. Dental insurance coverage for implants varies and is commonly limited.
Summary
Screwless and screw-based dental implants offer distinct design philosophies with implications for surgical approach, healing, maintenance, and aesthetics. Both types depend on successful osseointegration for long-term function. Choice of implant system in the United States in 2026 is influenced by patient-specific needs, clinical considerations, and cost factors. Ongoing research continues to evaluate comparative outcomes to guide evidence-based decisions in implant dentistry.