Early HIV Symptoms, Testing, and ART Guidelines 2026
Early HIV infection symptoms mimic common viral illnesses, so timely testing is crucial for diagnosis. Recognizing symptom patterns, adhering to U.S. HIV testing guidelines, and accessing antiretroviral therapy (ART) help improve health outcomes and reduce HIV transmission nationwide.
Recognizing Early HIV Symptoms
Acute HIV infection, typically occurring within weeks to months after exposure, may present symptoms resembling influenza or other viral illnesses. These symptoms usually appear within 2 to 6 weeks post-infection and can last for several days to a few weeks. Common signs include:
- Fever
- Fatigue
- Sore throat
- Swollen lymph nodes
- Rash
- Muscle and joint aches
- Headache
- Night sweats
- Diarrhea
Because these symptoms are nonspecific and mild in many cases, they often go unrecognized as related to HIV. Nonetheless, during this period, the viral load in the bloodstream is very high, increasing the potential for transmission. Awareness and clinical suspicion in the presence of these symptoms, especially with known risk factors, support early testing and intervention.
HIV Testing Guidelines in the United States (2026)
The Centers for Disease Control and Prevention (CDC) recommends routine HIV screening for all individuals aged 13 to 64 years at least once as part of standard medical care. For persons at higher risk, more frequent testing is advised, including:
- Men who have sex with men (MSM)
- People with multiple sexual partners
- Individuals with a history of sexually transmitted infections (STIs)
- Injection drug users or those who share needles
- Sex workers
- Partners of HIV-positive individuals
Testing after potential exposure is crucial. For example, anyone engaging in unprotected sex with partners of unknown HIV status or who share injection equipment should seek testing promptly. If considered for postexposure prophylaxis (PEP), testing and evaluation should occur within 72 hours of exposure. PEP is most effective when started as soon as possible, ideally within 24 hours.
Pregnant individuals are recommended to undergo HIV testing early in pregnancy to reduce the risk of perinatal transmission through appropriate management.
Types of HIV Tests and Window Periods
Several HIV diagnostic tests are available in the United States, each detecting infection at different stages post-exposure:
-
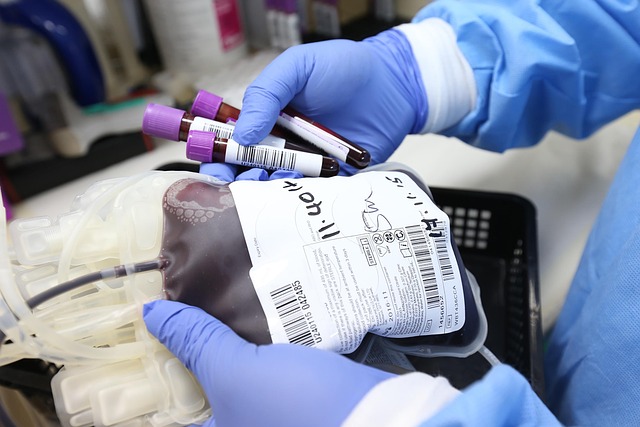
Nucleic Acid Tests (NATs): Detect HIV RNA in blood; can identify infection 10 to 33 days after exposure. These tests are more expensive and not routinely used unless recent exposure with symptoms or high suspicion exists.
-
Antigen/Antibody Tests: Use blood samples to detect HIV p24 antigen and antibodies; typically can detect infection 18 to 45 days post-exposure. These tests are common in clinical settings.
-
Antibody Tests: Detect antibodies to HIV in blood or oral fluid; generally have longer window periods (23 to 90 days).
Individuals with recent high-risk exposure and negative initial tests should consider retesting based on recommended intervals due to window periods.
Antiretroviral Therapy (ART) in HIV Management
Antiretroviral therapy involves the use of medications that suppress HIV replication, improving immune function and reducing mortality. Current U.S. guidelines recommend initiating ART as soon as possible after diagnosis, regardless of CD4 count.
Benefits of ART
- Improved Life Expectancy: Early ART reduces complications related to HIV and associated infections.
- Viral Suppression: ART reduces the amount of HIV in blood to undetectable levels, drastically lowering transmission risk.
- Reduced Morbidity: ART decreases the incidence of opportunistic infections and certain cancers.
ART Regimens
Modern ART regimens typically combine three antiretroviral drugs from at least two different drug classes. These classes include:
- Nucleoside/Nucleotide Reverse Transcriptase Inhibitors (NRTIs)
- Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs)
- Protease Inhibitors (PIs)
- Integrase Strand Transfer Inhibitors (INSTIs)
Regimen selection considers patient lifestyle, potential side effects, drug interactions, and resistance testing results.
Adherence and Monitoring
Consistent medication adherence is critical for achieving and maintaining viral suppression. Clinical monitoring includes viral load and CD4 count assessments, as well as evaluation for potential side effects and comorbid conditions.
HIV Prevention Strategies Related to Testing and ART
While testing and treatment form the foundation for individual and public health efforts, additional prevention measures include:
- Pre-Exposure Prophylaxis (PrEP): Medications taken by HIV-negative individuals at high risk to prevent infection.
- Post-Exposure Prophylaxis (PEP): Short-term ART started soon after potential exposure.
- Condom Use: Reduces transmission risk during sexual activity.
- Needle Exchange Programs: Reduces HIV transmission among injection drug users.
Typical Costs in United States (2026)
When considering HIV testing and treatment, typical price ranges vary depending on services and coverage:
- Basic Testing: Antibody-only rapid tests typically range from $20 to $50; some health departments provide testing free of charge.
- Standard Testing: Lab-based antigen/antibody and NAT tests generally cost between $50 and $150.
- Antiretroviral Therapy: Monthly medication costs vary widely; generic options may cost several hundred dollars per month, whereas brand-name regimens may exceed $2,000 monthly without insurance. Many patients access ART through public programs such as Ryan White HIV/AIDS Program or insurance.
Clinical visits, laboratory monitoring, and supportive services involve additional costs, which may be partially or fully covered by insurance, Medicaid, or assistance programs.
Summary
Understanding the early symptoms of HIV infection, following established U.S. testing guidelines, and accessing antiretroviral therapy are integral components of HIV management in 2026. Early diagnosis enables timely treatment initiation and helps prevent transmission. Testing technologies and treatment options have evolved, supporting improved outcomes for people with HIV across the United States.




